Nephritic syndrome
Table of contents
- Introduction
- Glomerular filtration barrier
- Aetiology of nephritic syndrome
- Clinical features
- Investigations
- Histopathology
- Management
- Prognosis
- Resources
Introduction
Nephritic syndrome is a clinical syndrome characterised by:
- Haematuria: visible or nonvisible, with dysmorphic red blood cells (e.g. acanthocytes) and RBC casts
- Sterile pyuria
- Proteinuria (<3.5g/24h)
- Hypertension
- Oedema
- Oliguria
- Uraemia
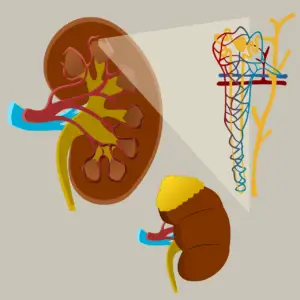
Glomerular filtration barrier
The glomerular filtration barrier is a highly specialised interface, that selectively allows passage of molecules based on size and charge. The GFB is composed of 3 layers:
- Glomerular capillary endothelium: The endothelial lining of glomerular capillaries is fenestrated, allowing movement of water, solute and large molecules, but preventing filtration of blood cells. Surrounding the luminal surface of endothelium is negatively charged glycosaminoglycans, which repel negatively charged molecules
- Glomerular basement membrane: composed of heparin sulphate, type IV collagen and laminin. The negatively charge of heparin sulphate repels negatively charged molecules such as albumin
- Bowman’s capsule visceral epithelium: Composed of podocytes, specialised epithelial cells that project foot processes. The foot processes interdigitate, forming filtration slits. The filtration slits are bridged by a thin diaphragm (the slit diaphragm) containing tiny pores.
In nephritic syndrome, inflammation and immunological injury to the glomerular filtration barrier allows red blood cells, white bloods, albumin and other large molecules to pass into the urine.
Aetiology of nephritic syndrome
- Post-streptococcal & Postinfectious glomerulnephritis
- Ig A nephropathy
- Rapidly progressive glomerulonephritis
- Antiglomerular basement membrane
- Anti-GBM disease when only glomerulus is involved
- Goodpasture syndrome when glomerular and alveolar basement membrane involved
- Immune complex mediated-conditions e.g.:
- Post-streptococcal glomerulonephritis
- IgA nephropathy
- Lupus nephritis
- Infective endocarditis
- Pauci-immune conditions
- Granulomatosis with polyangiitis (GPA, formerly Wegener’s granulomatosis)
- Microscopic polyangiitis
- Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)
- Antiglomerular basement membrane
- Mesangiocapillary (Membranoproliferative) glomerulonephritis
- Alport’s syndrome
Clinical features
Symptoms and signs of nephritic syndrome include:
- Haematuria: visible -> ‘coca-cola urine’ – or nonvisible
- Elevated blood pressure
- Oedema – periorbital, legs, sacral and signs of fluid overload
- Reduced urine output/Oliguria < 400ml/day
- Uraemia symptoms – nausea, fatigue, loss of appetite, pruritus
- Signs of underlying causes, e.g. fever, new murmur, rash
Investigations
Urine
- Urinalysis
- Haematuria
- Mild-moderate proteinuria
- Urine microscopy
- Dysmorphic RBC (acanthocytes)
- RBC casts
- Sterile pyuria
Bloods
- FBC
- U&E, eGFR
- LFT’s
- ASO titre
- Blood cultures
- Autoantibodies:
- ANA, Anti-dsDNA
- ANCA
- Anti-GBM
- Viral serology: Hepatitis B & C, HIV
- Serum complement levels (C3, C4, CH50)
Throat/skin swab culture
Radiological imaging
- Chest x-ray
- Renal ultrasound
Renal biopsy
Histopathology
- Poststreptococcal/Postinfectious glomerulonephritis
- Light microscopy: Acute diffuse proliferative glomerulonephritis; glomeruli are enlarged and hypercellular
- Immunofluorescence: granular deposition if IgG, C3, and, occasionally IgM in measangium and GBM in ‘starry sky’ pattern
- Electron microscopy: subepithelaial immune complex deposition
- IgA nephropathy:
- Mesangial proliferation and deposition of Ig A in mesangium
- Rapidly progressive glomerulonephritis
- Diffuse, proliferative, necrotising glomerulonephritis with crescent formation.
- Membranoproliferative glomerulonephritis
- Splitting of the GBM with interposition of mesangial cell cytoplasm between the endothelium and GBM is evident, giving a ‘tram-tracking’ appearance. Immunofluorescence shows subendothelial deposition of IgG.
- Alport syndrome: Thinning of GBM (early); Irregular GBM thin and thick areas with lamellation, giving a ‘basket weave’ appearance
Management
Management depends on the underlying cause:
- Poststreptococcal glomerulonephritis: usually self-limiting, supportive management with BP management and diuretics
- IgA nephropathy: Supportive with BP management and ACE-i/ARB; SGLT2 inhibitor; Steroids indicated for progressive renal impairment or persistent proteinuria
- Rapidly progressive glomerulonephritis:
- Corticosteroids: IV methylprednisolone, followed by oral prednisolone
- Immunosuppression: Cyclophosphamide; Rituximab is being increasingly used with success; Mycophenolate mofetil is indicated for SLE
- Plasmapheresis
- Renal dialysis
- Membranoproliferative glomerulonephritis: BP management, ACE-i/ARB; SGLT2 inhibitor
- Alport’s syndrome: BP management with ACE-i/ARB; Tolvaptan; Renal replacement therapy
Prognosis
Prognosis of nephritic syndrome is variable depending on underlying cause.
Poststreptococcal glomerulonephritis is usually self-limiting and prognosis is good – 90% resolve, <1% develop to rapidly progressive glomerulonephritis
Rapidly progressive glomerulonephritis
Resources
- Kumar & Clark’s Essentials of Clinical Medicine Seventh edition
- Oxford Handbook of Clinical Medicine 11th edition
- Medicine for MRCP Oxford Specialty Training
- TeachMePhysiology The Glomerulus – Structure – Filtration – TeachMePhysiology
- MedBullets: Nephritic Syndrome – Renal – Medbullets Step 2/3
- Miller M, Klinger M, Dziemianko I, Kazimierczak K, Drabczyk R. Rapidly Progressive Glomerulonephritis (RPGN). McMaster Textbook of Internal Medicine. Kraków: Medycyna Praktyczna Nephritic Syndrome – StatPearls – NCBI Bookshelf (nih.gov)