Nephrotic Syndrome
Table of contents
- Introduction
- The glomerular filtration barrier
- Aetiology of nephrotic syndrome
- Clinical features of nephrotic syndrome
- Investigations
- Histopathology
- Management
- Complications
- Resources
Introduction
Nephrotic syndrome is a clinical syndrome that results from increased permeability across the glomerular capillary wall to macromolecules due to structural and functional abnormalities of glomerular podocytes.
Nephrotic syndrome is defined by the triad:
- Heavy proteinuria: >3.5g/24h
- Hypoalbuminaemia: <30g/l
- Peripheral oedema
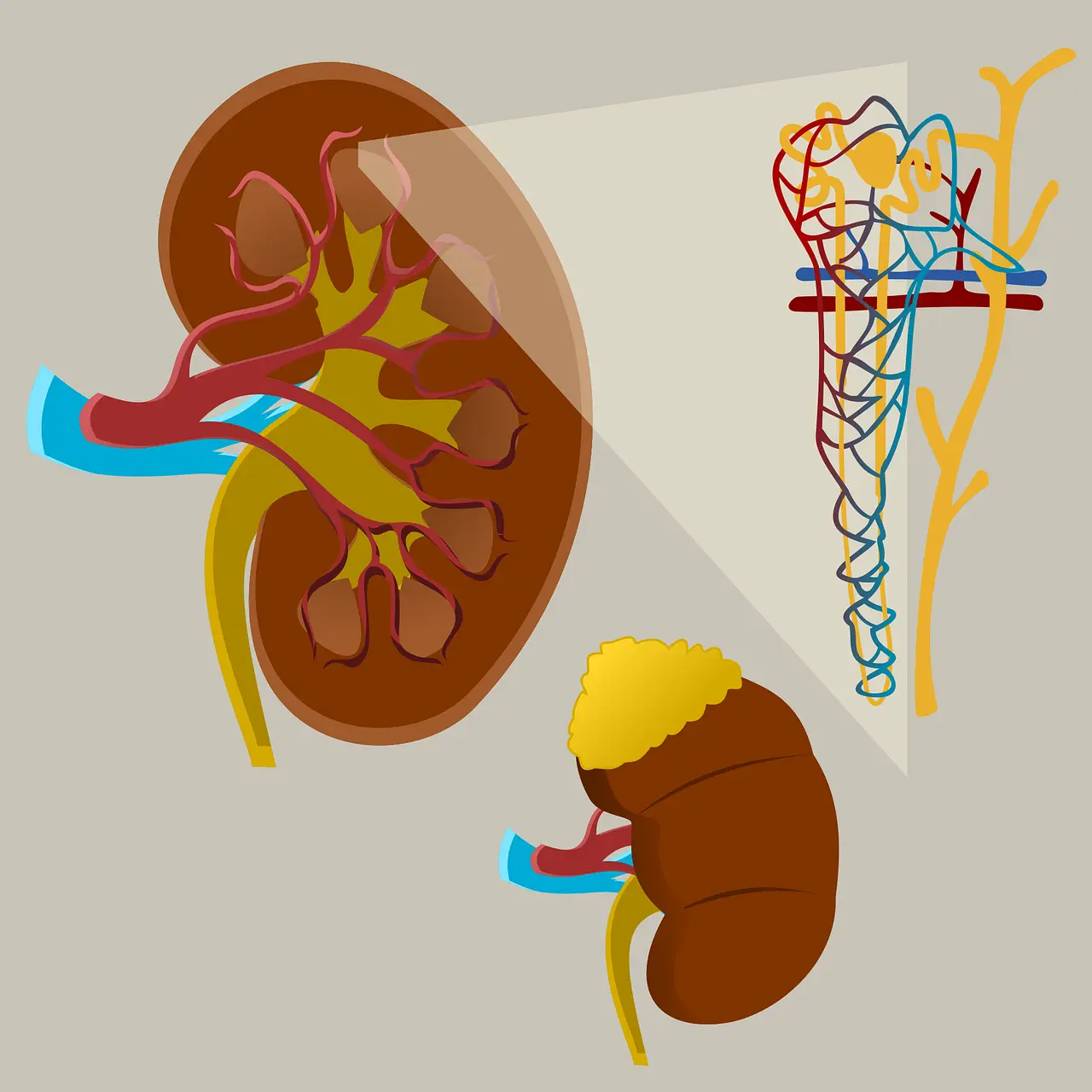
The glomerular filtration barrier
The glomerular filtration barrier is a highly specialised interface, that selectively allows passage of molecules based on size and charge. The GFB is composed of 3 layers:
- Glomerular capillary endothelium: The endothelial lining of glomerular capillaries is fenestrated, allowing movement of water, solute and large molecules, but preventing filtration of blood cells. Surrounding the luminal surface of endothelium is negatively charged glycosaminoglycans, which repel negatively charged molecules
- Glomerular basement membrane: composed of heparin sulphate, type IV collagen and laminin. The negatively charge of heparin sulphate repels negatively charged molecules such as albumin
- Bowman’s capsule visceral epithelium: Composed of podocytes, specialised epithelial cells that project foot processes. The foot processes interdigitate, forming filtration slits. The filtration slits are bridged by a thin diaphragm (the slit diaphragm) containing tiny pores.
In nephrotic syndrome, there is significant damage to podocytes or the slit diaphragm, resulting in failure of the glomerular filtration barrier. This allows albumin and other large molecules to pass into the urine.
Aetiology of nephrotic syndrome
Primary:
Intrinsic to the kidney and often idiopathic
- Minimal change disease
- Membranous nephropathy
- Focal segmental glomerulosclerosis
- Membranoproliferative/Mesangiocapillary glomerulonephritis
- Congenital nephrotic syndrome
Secondary
Associated with systemic conditions
- Diabetic nephropathy
- Amyloidosis
- SLE
- Malignancy
- Multiple myeloma
- Viruses: HIV, Hepatitis B & C
- Pre-eclampsia
- Drugs: NSAID’s, gold, penicillamine, bisphosphonates, lithium, interferon, heroin
- Henoch Schonlein Purpura
- Cryoglobulinaemia
Clinical features of nephrotic syndrome
Symptoms
- Fluid overload: facial oedema is common in children, followed by generalised oedema. Adults: dependent oedema in adults, weight gain, dyspnoea,
- Frothy urine: due to high protein content
- Nausea and anorexia
- Fatigue
- DVT or PE may be presenting feature due to thrombotic complications
- Recurrent infections due to impaired immunity
Signs
- Oedema
- Xanthelasma, Xanthoma due to associated hyperlipidaemia
- Pleural effusion
- Ascites
Investigations
Urine
- Urinalysis: 3+ or 4+ proteinuria. A 3+ reading represents at least 300mg/dl of protein, which correlates to daily loss of > 3.5g/d
- Urine microscopy
- 24 hour collection: is diagnostic
- ACR: protein:creatinine ratio 300mg/mmol is diagnostic
Blood:
- FBC
- Serum albumin, LFT’s
- U&E, eGFR
- Blood glucose
- Serum cholesterol & triglycerides
- Autoantibodies:
- Anti-nuclear antibodies, anti-dsDNA: for SLE
- ANCA
- Anti-PLA2-R: Phospholipase A receptor (PLA-R) is a transmembrane receptor expressed on the surface of podocytes. Autoantibodies against PLA-R are positive in ~70% of patients with idiopathic membranous nephropathy. Levels correlate with disease activity
- Complement levels – C3, C4, CH50
- Viral serology: HIV, Hepatitis B & C
- Serum electrophoresis
- Cryoglobulins
Radiology
- Chest XR
- Renal ultrasound
Renal biopsy
Histopathology
Minimal change disease: light microscopy show no change; immunofluorescent staining for immune complexes is negative; Diffuse effacement of podocytes is seen on electron microscopy
Membranous glomerulopathy: Diffusely thickened basement membrane; granular pattern on immunofluorescence; on electron microscopy immune complexes are subepithelial; a characteristic “spike and dome” appearance is visible on on silver staining, with membrane deposition growing around subepithelial immune complex deposition
Focal segmental glomerulosclerosis: Some glomeruli have scarring of certain segments i.e. focal sclerosis. Can be missed if < 10 glomeruli in biopsy sample
Mesangiocapillary (membranoproliferative) glomerulonephritis: Splitting of the GBM with interposition of mesangial cell cytoplasm between the endothelium and GBM is evident, giving a ‘tram-tracking’ appearance. Immunofluorescence shows subendothelial deposition of IgG.
Management
- Salt and fluid restriction to reduce oedema
- Loop diuretics – furosemide; thiazide diuretic may be added if resistant
- ACE-i/ARB to reduce proteinuria
- Specific therapy depends on underlying cause. Corticosteroids e.g. prednisolone are the mainstay. 10-20% are steroid resistant and 50% more likely to progress to ESRD. Immunosuppressant therapy e.g. cyclophosphamide is required.
- Anticoagulation in selected patients
Complications
- Hyperlipidaemia: Hyper-cholesterolaemia and triglyceridaemia is thought to be due nonselective increase in lipoprotein synthesis by the liver in response to a decrease in oncotic pressure, and to impaired lipid breakdown due to lipoprotein lipase deficiency
- Thromboembolism: hypercoagulability is multifactorial, due to renal loss of antithrombin III, increased hepatic synthesis of clotting factors, and platelet abnormalities
- Recurrent infections: renal loss of immunoglobulins and immune mediators; oedema acts a focus of infection
- Hypovolaemia
- AKI: more commonly precipitated by hypovolaemia and sepsis or renal vein thrombosis
Resources
- Kumar & Clark’s Essentials of Clinical Medicine Seventh edition
- Oxford Handbook of Clinical Medicine 11th edition
- Medicine for MRCP Oxford Specialty Training
- TeachMePhysiology The Glomerulus – Structure – Filtration – TeachMePhysiology
- Tapia C, Bashir K. Nephrotic Syndrome. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: Nephrotic Syndrome – StatPearls – NCBI Bookshelf (nih.gov)
- Hashmi MS, Pandey J. Nephritic Syndrome. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562240/
- Medscape Nephrotic Syndrome: Practice Essentials, Pathophysiology, Etiology (medscape.com)